friends how you saved my life!”

long enough to get a new liver!”

the very best treatment and advice.”

kind and genuinely caring”
We schedule outpatient interventional radiology procedures performed at the Salem Hospital.
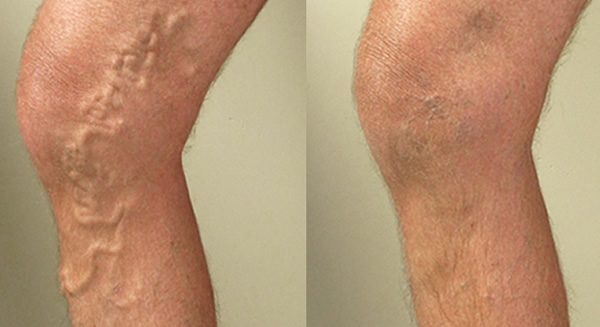
Free Vein Screening
Tired, Achy, Swelling Legs? Bulging Veins or Ulcers? We can help. Schedule a FREE Consultation.
Call to Schedule
Our team is ready to answer your questions and schedule your appointment. Give us a call.
- INTERVENTIONAL RADIOLOGY
- ABSCESS & FLUID DRAINAGE
- BIOPSY
- CATHETER, LINE AND PORT PLACEMENT
- DIALYSIS CARE
- DVT & PE THROMBOLYSIS
- GASTROSTOMY TUBES
- GENITOURINARY & UROLOGICAL
- HEPATOBILIARY
- IVC FILTER
- KYPHOPLASTY / VERTEBROPLASTY
- PAIN INJECTIONS & NERVE BLOCKS
- PARACENTESIS / THORACENTESIS
- PELVIC CONGESTION SYNDROME & VARICOCELE
- TUMOR EMBOLIZATION & ABLATION
- UTERINE FIBROID EMBOLIZATION
- VARICOSE VEINS
- VASCULAR
- VASCULAR EMBOLIZATION
Interventional Radiology
Our interventional radiology team provides minimally-invasive treatments as an alternative to open surgery. Interventional radiology procedures may reduce risk, pain and recovery time. Patients are treated non-surgically by placing a catheter inside the body with image-guided technology such as Computed Tomography (CT) Scans, X-rays and Magnetic Resonance Imaging (MRI).
Our experienced care team performs ablation for isolated metastases to the liver, lung, adrenal gland, bone, kidney and other soft tissues. Liver metastases can be treated with Yttrium-90 radioembolization and chemoembolization. Radio Frequency Ablation (RFA) and Microwave Ablation may damage the cancerous tissue itself and Transarterial Chemoembolization can cut off the blood supply to a tumor.
Interventional radiology may be used in the management of metastatic cancer diseases such as colorectal, breast, gallbladder, pancreas, lung, esophageal, stomach, melanoma and sarcomas.
Abscess and Fluid Drainage
Biliary Drains
Bile is a digestive fluid your liver produces to break down fats for better absorption by the body. It is stored in the gallbladder and flows from the liver through the bile ducts to the small intestine (duodenum). Several conditions can cause the narrowing or obstruction of the bile ducts–called a biliary obstruction–including gallstones, trauma, cysts or tumors, pancreatitis, injuries, and infections.
When the duct is obstructed, bile can back up and collect in the liver, causing complications such as infection, nausea, vomiting and jaundice. A biliary drain can be placed above the blockage to drain the bile from the liver through a tube or catheter and into a drainage bag outside the body that patients manage at home.
Our interventional physicians and physician assistants often work with biliary drains, either to place them, adjust them, or replace and remove them.
Biopsy
Our Interventional Radiologists and/or physician assistants perform the following types of biopsies:
Liver, lymph node, renal, lung, thyroid, bone marrow, bone lesion, and soft tissue masses. During a biopsy a small piece of tissue is taken from the area in question using a specialized biopsy instrument. Tissue samples are preserved and sent to pathology for diagnosis. Your ordering physician will be notified of the results via the pathology department report.
Some biopsy procedures require some slight sedation to help you relax during the procedure and may require the placement of an IV. All biopsies are fairly quick and once you have recovered, you will be discharged the same day.

Catheter, Line and Port Placement
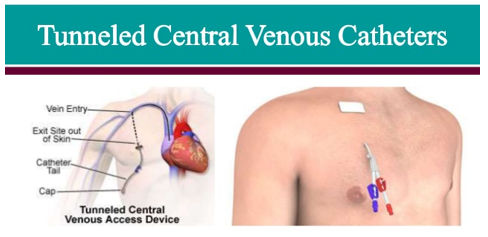
Tunneled Catheter Placement
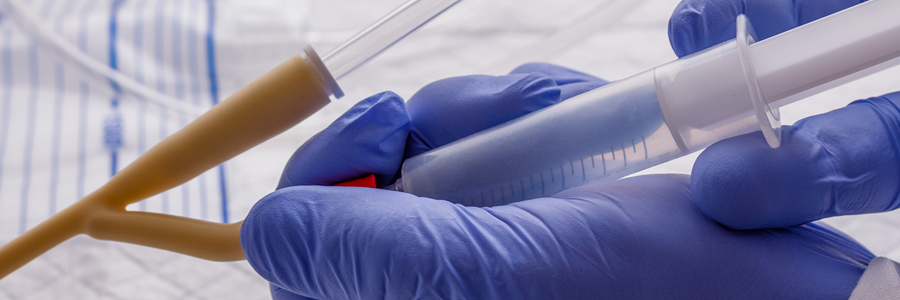
A catheter is a thin, long, flexible tube placed in a vein that is designed to deliver medication, take blood samples, provide nutrition, and avoid multiple needle sticks over an extended period of time. A tunneled catheter is also called a central line. It is most commonly placed in the neck, but could also be placed in the groin, liver, chest, or back, and is very secure in the vein. Our radiologists insert and remove these types of catheters.
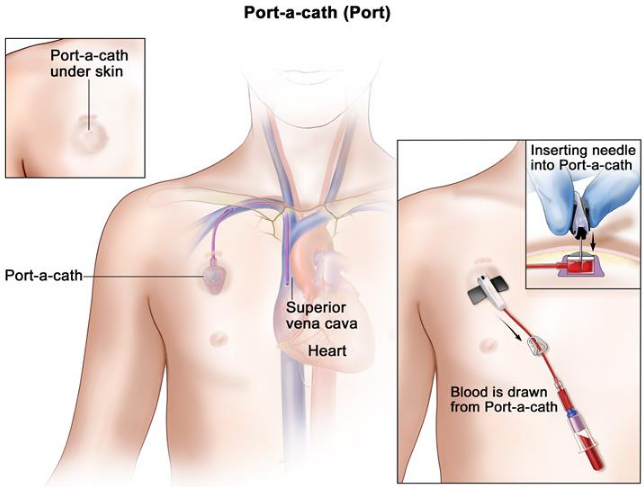
Power Port
A Power Port is small, portable, light weight implantable device that is commonly used for patients requiring repeated injections of medicine into the bloodstream. It also can be used as an access point for recurring blood draws or for injecting contrast that is administered with many radiology procedures. With a power port, patients avoid the pain and discomfort associated with multiple needle sticks.
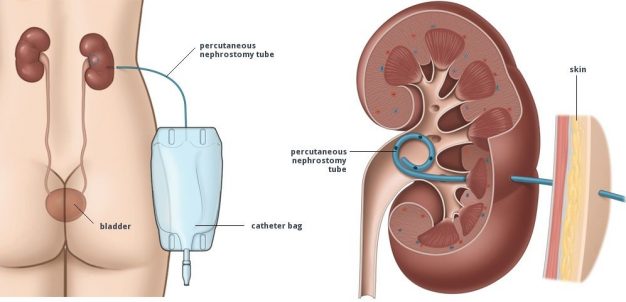
Percutaneous Nephrostomy Tube Placement
Percutaneous nephrostomy tube placement is a procedure using a catheter to drain urine from the body into a collecting bag. The radiologist will use imaging to guide a needle into the kidney and inject dye to better visualize the kidney. The needle is then replaced by a soft catheter that stays in the kidney to drain urine into a collection bag outside the body.
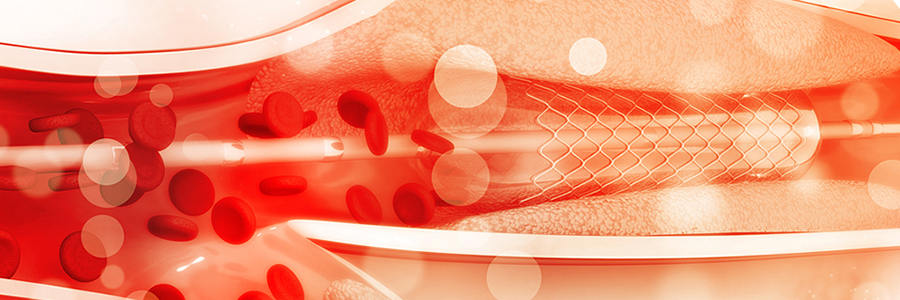
Fistula Repairs
A fistula is created by surgically joining a section of an artery and a vein to make a larger vessel capable of flowing high volumes of blood during hemodialysis. Occasionally a fistula may become clogged or narrowed which prevents further dialysis treatments until resolved.
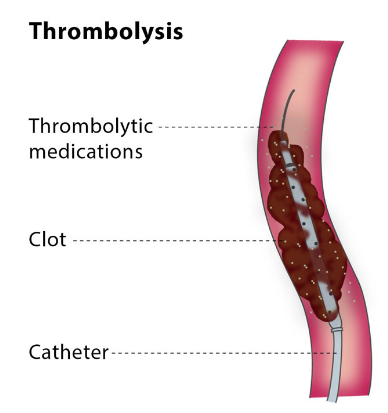
When this occurs, an interventional radiologist will use image guided interventions to re-open the flow of blood through the blocked fistula. The interventional radiologist will typically use a procedure called thrombolysis or another procedure called angioplasty and stenting to repair the fistula.
With thrombolysis, a catheter is inserted into an artery or vein and directed to the area of narrowing. The blockage is then dissolved by using medication or a mechanical device to break up the clot. With angioplasty and stenting, a mechanical device such as a balloon will be inserted and expanded to enlarge the area of narrowing and in some cases, a mesh tube (stent) may be inserted to help the vessel remain open.

Dialysis Care
Fistulogram
A procedure used to visualize a fistula using contrast and fluoroscopic x-ray.
DVT & PE Thrombolysis
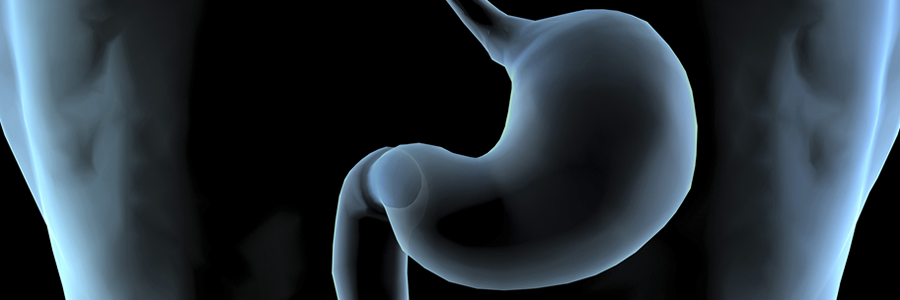
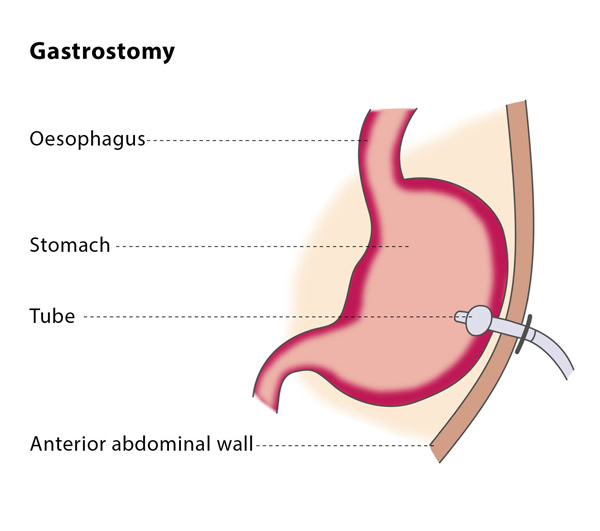
Gastrostomy Tubes
Certain medical problems prevent individuals from obtaining adequate nutrition by mouth. A gastrostomy tube (also called a G-tube) is a soft, narrow tube inserted through the upper part of the abdomen that delivers nutrition and medications directly to the stomach. This allows individuals with trouble eating, to get the fluid and calories they need. The same tube can also be used to drain fluids from the stomach. The tube can be left in place for 3-6 months depending on the type of tube that is placed and then is exchanged or removed by an interventional radiologist.

Genitourinary & Urological
Percutaneous Nephrostomy
A procedure to place a tube directly through the skin into the kidney for drainage.
Hepatobiliary
Transjugular Intrahepatic Portal System Shunt (TIPS)
A method to divert blood from the liver using an intravenous catheter.
Percutaneous Transhepatic Cholangiogram
A procedure to visualize the liver and gallbladder using contrast and fluoroscopy.
IVC Filter
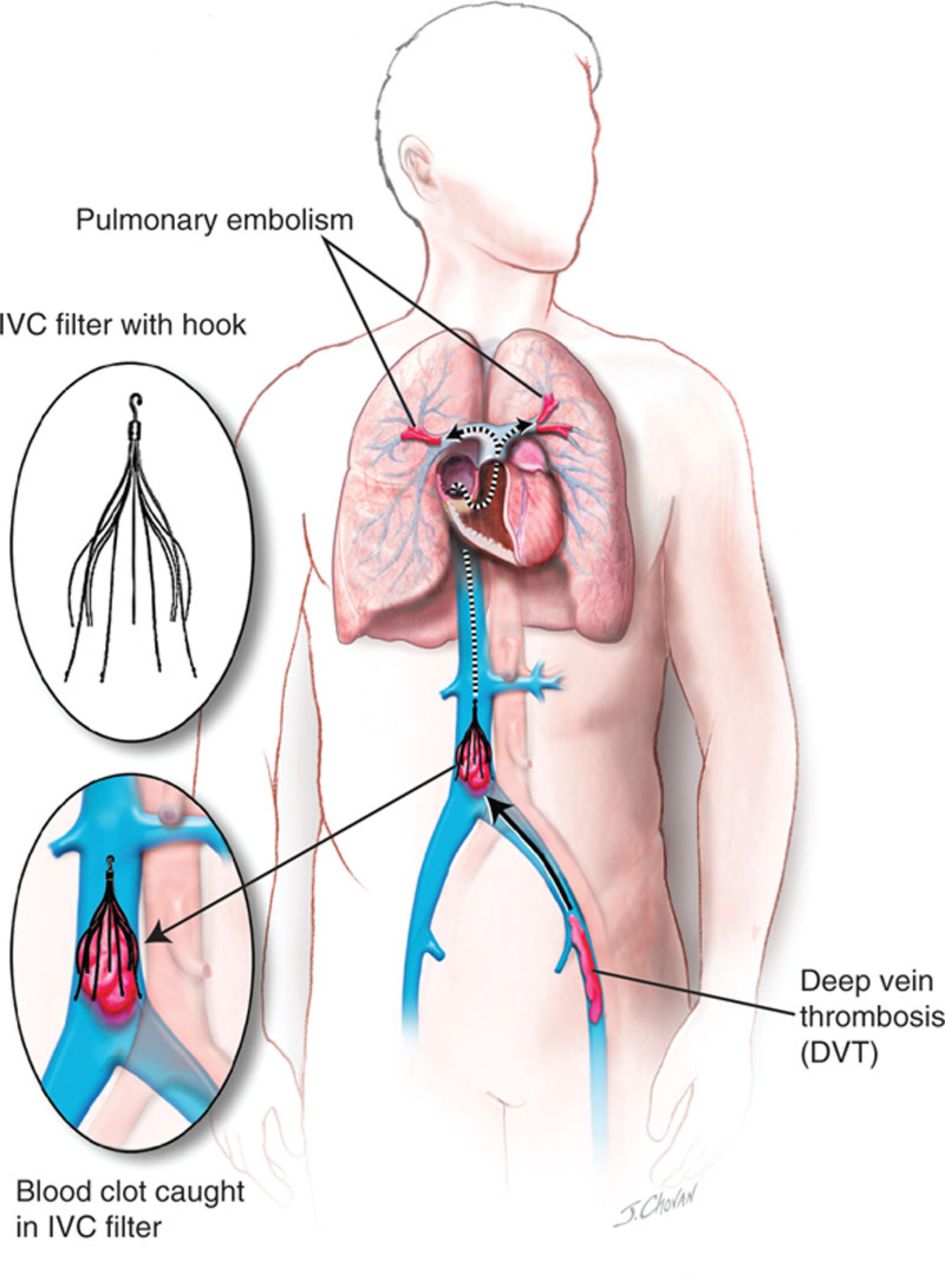
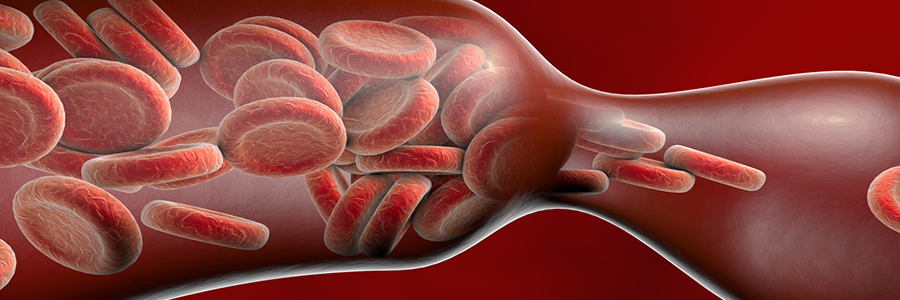
The inferior vena cava (IVC) is the large vein in the abdomen that returns blood from the lower body to the heart. An IVC filter is a small metal device that is placed in this vein to prevent blood clots that form in the legs or pelvis from reaching the lungs or heart. These blood clots are known as deep vein thrombosis, or DVT.
For this procedure, our radiologist places the filter in a very small catheter and uses imaging guidance to access the vein and carefully place the filter, which traps the clot fragments and keeps them from traveling through the IVC to the heart and lungs where they can cause severe complications.
IVC filters are designed to be temporary and can be removed from the vein when the risk of a clot moving to the heart or lungs has passed. Removing the filter eliminates any long-term risks of keeping it in place, but does not address the cause of DVT. Your referring doctor will decide if blood thinners are still necessary. Not all filters should be removed, such as when the risk of clots persists or blood thinners are not an option.
Below is a diagram to help you better understand how the filter works. In the inset pictures, you can see what the filter looks like and how it traps a clot and prevents it from moving further up the vein.
Kyphoplasty / Vertebroplasty
Spinal fractures occur when one of the bones in the spine fractures or collapses. Cancer, chemotherapy, hyperthyroidism, injury and long-term use of corticosteroids contribute to bone loss, as do more common conditions such as osteoporosis, menopause.
Kyphoplasty and vertebroplasty are procedures used to treat spinal fractures. Both are same-day procedures involving minimally invasive incisions and very little healing time.
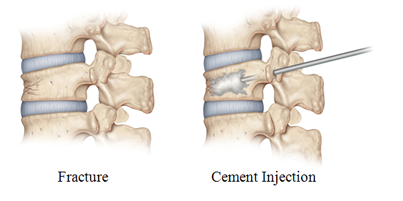
During a kyphoplasty procedure, a space is created within the fractured bone by a balloon-tipped catheter. The catheter is placed by using imaging guidance. The balloon is inflated to make space for liquid bone cement, which is then injected. The cement hardens in about ten minutes. The goal of the procedure is to relieve the pain being caused by spinal compression. Patients may experience a dramatic reduction in pain following the procedure.
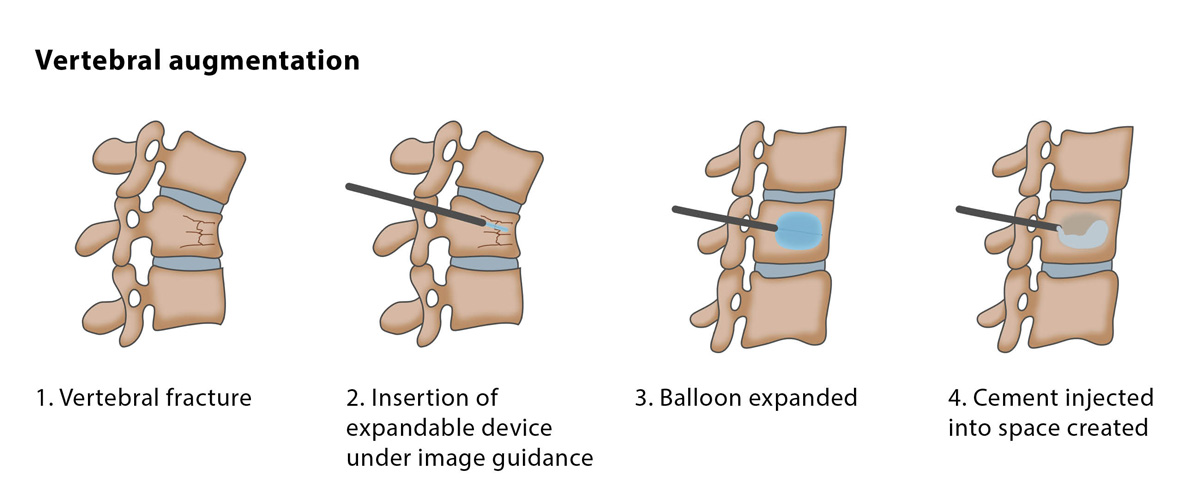
Vertebroplasty is similar and also helps stabilize the fracture, fuse any bone fragments, and relieve the pain. To perform the procedure, a radiologist will use imaging to guide a needle into the fractured vertebrae itself, and inject a bone cement mixture, which hardens in roughly ten minutes. Patients can typically return home the same day.

Pain Injections & Nerve Blocks

Paracentesis / Thoracentesis
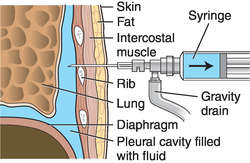
Thoracentesis
Thoracentesis is a procedure performed to remove excess fluid buildup between your lungs and chest wall, known as the pleural space. Normally there are about 4 teaspoons of fluid in the pleural space, but some conditions cause that amount to increase. Heart failure, lung infections, and tumors are examples of things that can increase the amount of fluid in the pleural space and cause pressure on the lungs, making it hard to breathe. This is called a pleural effusion.
The interventional radiologist or physician assistant uses ultrasound equipment to guide a needle into the fluid in the pleural space and draw it out, relieving the pressure. This is a clinic procedure. Breathing can improve and patients can become more comfortable after the procedure.
Paracentesis
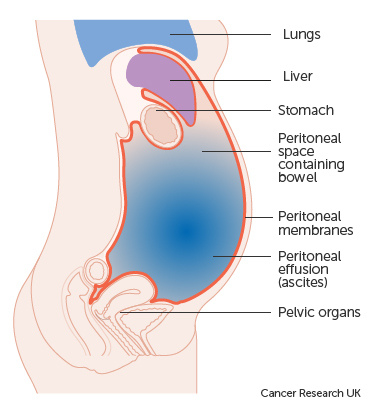
Paracentesis is a procedure to remove extra fluid that has collected in the belly region, specifically below the ribs and lungs and above the hips. This buildup is called ascites and can be caused by infection, inflammation, an injury, cancer, or cirrhosis, among other conditions. It can cause a number of symptoms, including pain, swelling, difficulty sitting, a feeling of sickness, loss of appetite, indigestion, and shortness of breath.
Paracentesis is performed by using ultrasound to identify the safest location to extract the fluid. The radiologist or physician assistant will numb the area first, then insert a needle into the abdominal cavity where the fluid is and place a catheter to drain the fluid. Once completed, paracentesis can relieve pressure and pain in the abdomen.
This is a procedure that can be scheduled and completed in our outpatient clinic.
How can I be seen at the IR Clinic?
Patients are typically referred by their PCP or specialist, such as a gastroenterologist or oncologist. Our knowledgeable and caring staff will call the patient and schedule a consultation appointment.
When you first arrive for your visit, we will perform vital measurements such as blood pressure, temperature, weight and height and review any prior lab and imaging tests. The physician assistant and the interventional radiologist will come in to discuss your health situation and go over the lab and imaging in detail with you so you have a good understanding of the diagnosis. Together with you, the best plan of action or treatment will be determined.
Any procedure questions or general questions about our Interventional Clinic can be directed to 503-763-7471 Monday-Friday 8am-4:30pm.

Pelvic Congestion Syndrome & Varicocele
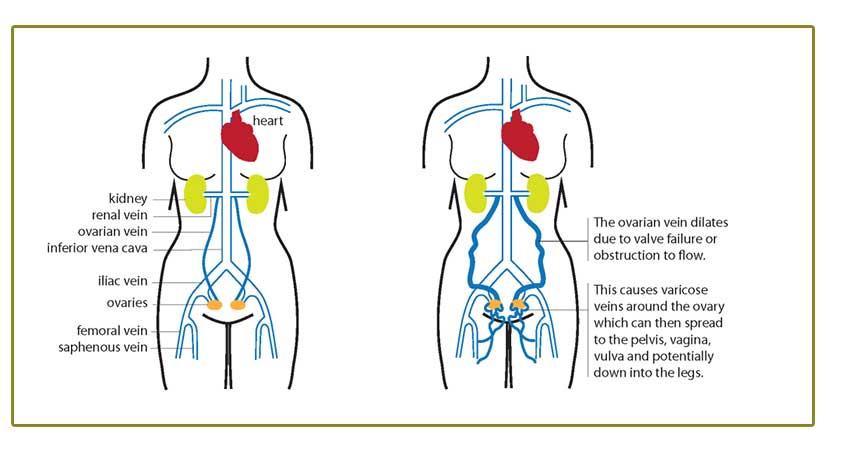
Chronic pelvic pain is a very common problem among women. Pelvic congestion syndrome (PCS), also known as pelvic vein incompetence, is a common cause of chronic pelvic pain in women. It is caused by varicose veins in the lower abdomen. PCS is similar to varicose veins in the legs, in that valves in the veins become weakened and no longer close properly, preventing blood from returning to the heart. Instead, blood flows backwards and pools in the veins, causing pressure, pain, and bulging veins.
In the pelvis, varicose veins can affect the uterus, ovaries, and vulva. Pain can be a dull ache, or can be sharp or throbbing, and can be aggravated by standing. In fact, the diagnosis can easily be missed because a pelvic exam is performed lying down, which relieves the pressure from the veins so they no longer exhibit symptoms.
Once a diagnosis is made via an ultrasound or other imaging test, an interventional radiologist can perform an embolization to treat the problem. This is a minimally invasive procedure which uses guided imaging to direct a small catheter to the problem area and intentionally plug the varicose vein and seal it with tiny coils or glue-like liquids. After this embolization procedure, patients can return to normal activities very quickly.

Tumor Embolization & Ablation
Salem Interventional Radiology performs a range of vascular embolization procedures. Please read below for a description of the following tumor embolization and ablation procedures:
- Transarterial Chemoembolization (TACE)
- Yttrium-90 (Y-90)
- Uterine Artery Embolization (UAE)
- Pelvic Congestion Treatment
- Pulmonary Arteriovenous Malformation Treatment
Transarterial Chemoembolization (TACE)
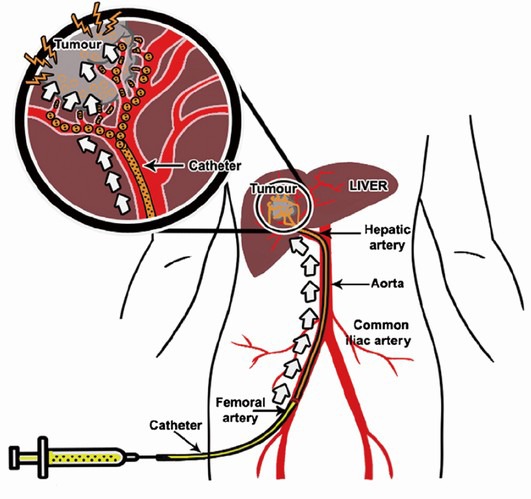
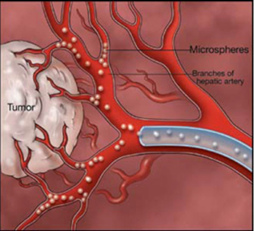
Patients receive TACE to treat cancerous tumors in the liver. TACE is a minimally invasive procedure performed using a catheter and imaging guidance to deliver tiny beads of chemotherapy medication (also known as embolic materials) into the arteries feeding the tumor. Embolic materials are those that intentionally lodge in the blood vessel and prevent blood flow to a tumor. The beads of chemotherapy medication serve to both block the blood supply from reaching the tumor, as well as provide the chemotherapy drugs directly to the tumor..
This is an out-patient procedure. Patients may experience flu like symptoms for approximately one week, and an increase in fatigue and general lack of energy for slightly longer. TACE can be performed multiple times to achieve the effect desired.
In the diagram, the small spheres in the round picture represent the embolic material cutting off the blood supply to the tumor.
Y90 – Yttrium-90
Yttrium-90 or more commonly referred to as Y90 is an embolization therapy that involves two separate procedure appointments. During the first appointment the doctor will create a map of your blood vessels to evaluate if the procedure can be performed safely on you. The second appointment is the actual procedure during which there is administration of radiation directly to the liver tumor via a catheter. With this technique, the radiation is delivered in the form of tiny glass or resin beads filled with the radioactive isotope yttrium Y-90. These resin beads are placed inside the blood vessels that feed a targeted tumor. Because the radiation is delivered in a targeted manner directly at the site of the tumor, patients may avoid many of the side effects of traditional radiation therapy.
With the delivery of the radiation “beads”, your doctor will restrict the blood supply feeding the tumor. In this manner, the tumor is treated using two different techniques. If necessary, Y90 can be performed multiple times to achieve the desired response in the tumor.
After The Procedure: The hospital will send you home with aftercare instructions
You may have flu like symptoms for 5-10 days. This can begin a day after the procedure and last 7-10 days. Our office will be periodically check-in with you by phone after you have returned home from the procedure. Expect to feel very tired following the procedure and obtaining adequate rest is an important part of the recovery process.
The doctor will want you to get a blood draw 2 weeks after the procedure. We will send an order to the most convenient lab station. We will also have you get a CT Scan or MRI one month after treatment. This will be based on the doctor’s decision and the timeline could change, but our office will keep you informed. You are always welcome to call the office directly at 503-763-7471 with any questions. Our office hours are 8am-4:30pm M-F.
CT/US Guided Microwave Liver Ablation (also referred to as Radiofrequency Ablation or RFA)
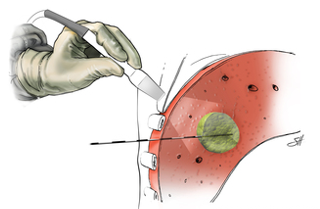
Another minimally invasive procedure our interventional radiologists use to treat cancer is microwave ablation (MWA). This is technology that uses a CT scan or ultrasound to place a needle or probe through the skin into a tumor. The needle then generates microwave energy and creates a small region of heat, which destroys the tumor cells.
Cryoablation
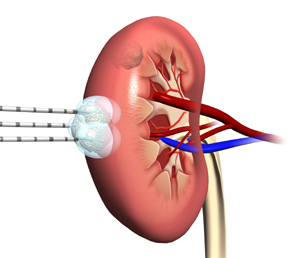
Cryoablation is an outpatient procedure that uses extremely cold temperatures to destroy abnormal cells, including kidney tumors. Also called cryotherapy or cryosurgery, it is a minimally invasive treatment that allows for very precise targeting of extreme cold to efficiently destroy abnormal cells, while leaving the nearby healthy tissue intact. Cryoablation is often used to treat different benign and cancerous tumors, and is favored as an alternative to a high-risk open surgery.
The radiologist uses a CT scan to guide the introduction of a cryoprobe into the tumor to freeze the tissue.
How can I be seen at the IR Clinic?
Patients are typically referred by their PCP or specialist, such as a gastroenterologist or oncologist. Our knowledgeable and caring staff will call the patient and schedule a consultation appointment.
When you first arrive for your visit, we will perform vital measurements such as blood pressure, temperature, weight and height and review any prior lab and imaging tests. The physician assistant and the interventional radiologist will come in to discuss your health situation and go over the lab and imaging in detail with you so you have a good understanding of the diagnosis. Together with you, the best plan of action or treatment will be determined.
Any procedure questions or general questions about our Interventional Clinic can be directed to 503-763-7471 Monday-Friday 8am-4:30pm.

Uterine Artery Embolization also referred to as Uterine Fibroid Embolization
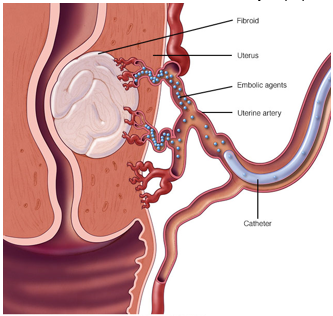
A growing, non-surgical option for treating uterine fibroids is uterine artery embolization (UAE). Uterine fibroids are very common, non-cancerous growths on or just outside the uterus. These fibroids range in size. They can cause heaving bleeding and prolonged menstrual periods, bloating, fullness, or pain in the belly/pelvis region, constipation, and pain. Fibroids occur in 20-40% of women older than 35.
UAE is a minimally invasive procedure performed by an interventional radiologist using imaging guidance during which a catheter is threaded through the blood vessels to the arteries supplying blood to the fibroids. Very tiny particles are injected that stick to the vessel walls, causing a clot to develop and block the blood supply to the fibroid. The desired outcome is that the fibroid begins to slowly shrink over time, which relieves or reduces the major symptoms.

Varicose Veins
Over 25 million Americans suffer from varicose vein disease. This is a debilitating disease process that is commonly thought of as a cosmetic disease, however we have learned that the cosmetic effects are just symptoms of something much more serious and life limiting. The reality is that men and women all across this country suffer from severe symptoms related to the underlying cause of varicose veins due to a medical condition called superficial venous insufficiency.
Superficial venous insufficiency is a disease involving the surface level veins in the legs. The root of the disease is a malfunction of the “one-way” valves in the veins. These valves are designed to let blood travel one direction from the legs up to the heart and prevent the blood from traveling back down toward the feet. In many people these valves grow weak over time and become insufficient. This insufficiency allows blood to pool in the veins of the legs which creates symptoms of pain, “heavy” legs and fatigue. Over time the pressure leads to visible bulging veins in the legs and eventually can lead to a breakdown of the skin with open sores that resist healing and ulceration.
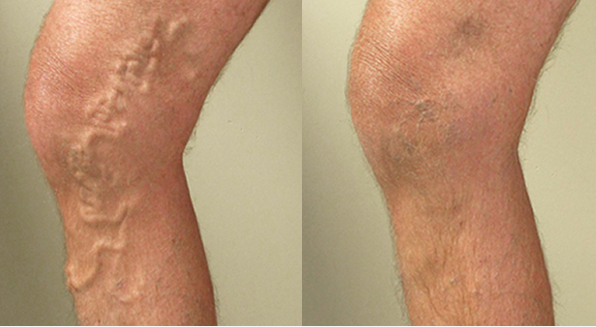
Treatment of superficial venous insufficiency is important to alleviate the life-limiting symptoms that many patients develop. Treatment will also delay and sometimes reverse the development of overlying visible changes. State of the art treatment of venous insufficiency begins with identifying the source of the problem with ultrasound. Once an appropriate source has been identified, the next step in treatment will usually be a trial of compression stockings. Wearing compression stockings provides the opportunity to evaluate how the patient may respond to treatment, but does not provide a permanent cure. The next step is typically to thermally treat and seal or ablate the diseased vein using minimally invasive catheter techniques. These techniques have nearly replaced traditional “stripping” surgery performed in the past for varicose veins. Minimally invasive techniques provide the same outcome as traditional surgery with minimal pain and minimal recovery time. The procedure is performed as an outpatient and patients can return to work the next day.
There are two other procedures that are often used in conjunction with thermal ablation technique, they are microphlebectomy and sclerotherapy. Microphlebectomy uses micro-incisions to remove problematic varicose veins which are the result of the underlying insufficiency. This is typically done after the underlying cause has been treated with thermal ablation. Sclerotherapy can be used for small veins that cannot be treated with phlebectomy or thermal ablation.
Patients interested in treatment are evaluated clinically and with ultrasound to determine the source of the venous insufficiency. Following evaluation a treatment plan is developed based on the specific anatomy and type of veins needing treatment. Treatment typically occurs in several stages requiring up to 8 months for the entire process to be completed. However, patients will begin to notice symptomatic improvement within a few weeks after the first treatment.
The full spectrum of minimally invasive varicose vein treatment is being offered by the interventional radiologists at the Salem Interventional Radiology clinic.
Vascular
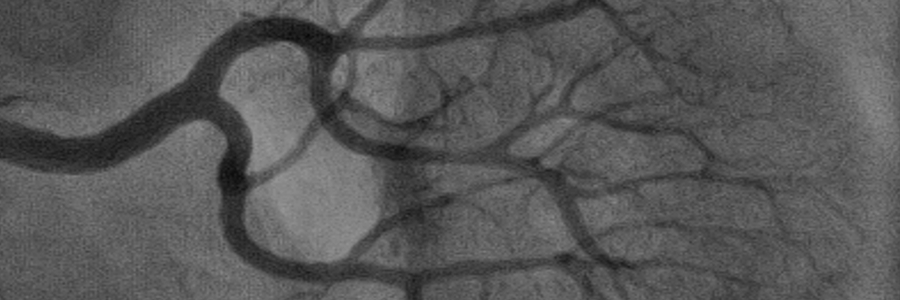
Angiogram (Carotid)
A procedure using x-ray examination via catheter placement in the carotid arteries to check for a narrowing or blockage.
Angiogram (Pulmonary)
A procedure to visualize the pulmonary artery using contrast and fluoroscopy.
Angiogram (Renal): A procedure to visualize the renal arteries using contrast and fluoroscopy.
Angiogram (Visceral)
A procedure to visualize the viscera using contrast and fluoroscopy.
Angiogram (Cerebral)
A procedure to visualize the cerebral arteries using contrast and fluoroscopy.
Angioplasty (Peripheral)
A procedure using a balloon catheter placed in a peripheral artery to open a blockage of the artery.
Angioplasty (Renal)
A procedure using a balloon catheter placed in the renal artery to open a blockage of the artery.
Venogram (Upper Extremity)
A procedure to visualize the upper extremity veins using contrast and fluoroscopy.
Venogram (Upper Extremity)
A procedure to visualize the upper extremity veins using contrast and fluoroscopy.
Venogram (Renal)
A procedure to visualize the renal veins using contrast and fluoroscopy.
Venogram (Lower Extremity)
A procedure to visualize the lower extremity veins using contrast and fluoroscopy.
Venacavagram
A procedure to visualize the vena cava using contrast and fluoroscopy.
Extremity Arteriogram
A procedure to visualize the arteries of an extremity using contrast and fluoroscopy.
Vascular Embolization
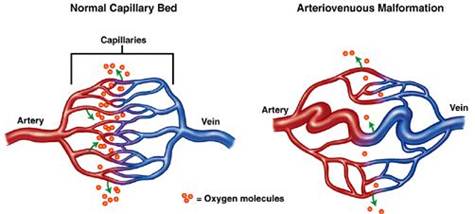
Coil Embolotherapy for Pulmonary Arteriovenous Malformations
Arteriovenous malformations are abnormal vascular connections between an artery and a vein. When this occurs in the lungs between the pulmonary vein and the pulmonary artery, it is called a pulmonary arteriovenous malformation, or PAVM. The malformation paradoxically means that there is increased blood flow through the area, but not as much oxygen reaching the blood, which can mean shortness of breath or heart failure as the heart works harder to compensate for the lack of oxygen. In addition, the PAVM can have weakened walls, leading to blood collecting around the lung or the coughing up of blood. Another serious complication includes higher risk of stroke or brain abscess, as small clots that would otherwise be trapped in tiny vessels are allowed to continue on through the PAVM to the vessels of the brain.
Depending on the size of the PAVM, a coil embolotherapy procedure can be used to block the arteries feeding the PAVM. This technique advances a steel coil using imaging guidance and contrast dye through a small catheter inserted in the groin area. After carefully working the catheter to the area of concern, the radiologist will place the coil outside the PAVM. The straightened coil will revert back to a spiral when released from the catheter, effectively obstructing the enlarged artery. Then the catheter will be removed. Sometimes more than one coil will be used during the procedure.
Salem Interventional Radiology
We are proud to be the largest radiology group in the Salem Oregon area. We offer a depth of specialization among our doctors that you would expect to find only at major university medical centers.
We are solely owned by a group of local radiologists whose mission is simply to provide the highest quality of patient care. In addition to the work we do onsite at our imaging facility, we also partner with local and regional hospitals and clinics to provide specialized radiology services.